The overmedication of American seniors.
Sabina King on Feb 5th 2020
The United States is currently suffering a largely underreported epidemic – the overmedication of its elderly population. Why this doesn’t get as much press as, say, the opioid epidemic, could be in part because issues relevant to seniors are seen as peripheral to mainstream healthcare. It could also be because the epidemic is still poorly understood. So how did this problem – also called polypharmacy – get so rampant in the first place? And how do we fix it?
What is polypharmacy? 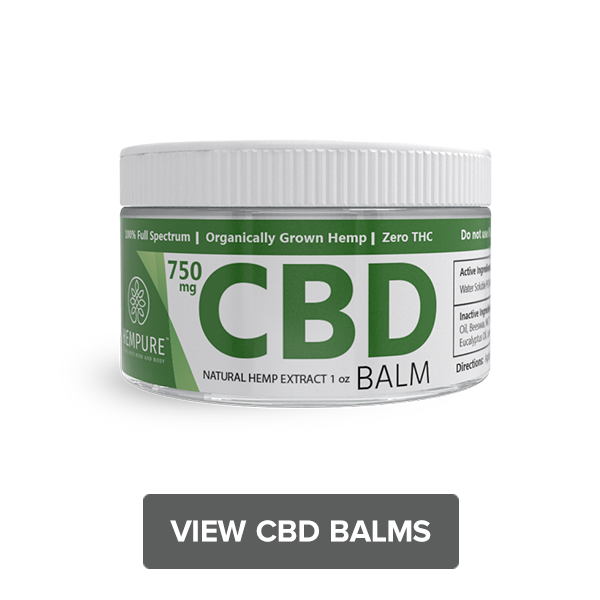
In simple terms, it’s the simultaneous or concurrent use of multiple medications. It’s most common among the elderly - the number of senior patients on multiple medications is steadily increasing. These medications are ostensibly prescribed to treat or manage conditions, but there is an inherent risk of drug interactions and side effects.
What are the dangers of polypharmacy or a ‘medication overload’?
Adverse drug events or ADEs as they are referred to in medical literature can include anything from confusion and falling to bleeding and respiratory problems.[1] Drug-related complications add about 3 days on average to hospital stays among senior populations.
Scarier still is the fact that polypharmacy has also been linked to unnecessary and premature death.[2] Older patients are more susceptible to these risks because their systems have a harder time metabolizing medicine.
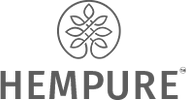
What do the numbers say about polypharmacy?
An extensive report by the Lown Institute brought to light some sobering statistics[3]:
Every day, 750 American seniors (aged 65+) are hospitalized due to serious side effects from one or more medications.
Over the last 10 years, seniors sought medical treatment more than 35 million times for adverse drug events, and there were more than 2 million hospital admissions.
Over the next 10 years (at the current rate of prescriptions) medication overload could contribute to the premature deaths of 150,000 older Americans, and impact the quality of life for millions more.
The reduction of inappropriate or unnecessary medications could save as much as $62 billion over the next decade, a sum based on the current rate of unnecessary hospitalizations.
Nearly 20 percent of American seniors take 10 or more prescription drugs a day.
Why does polypharmacy occur?
Let’s be clear – it’s very likely that doctors don’t want their elderly patients dying. The mechanism behind overmedication is often more insidious.
Excessive interest in prescription medication.
Advertisements for prescription drugs often appeal to the senior population, and many consistently link the use of these drugs to happier, fuller lives. Moreover, there is an increased need to ‘treat’ what are in fact natural milestones in the human aging process. Medical practitioners often feel compelled to do something to ease concerns that senior patients might have. More often than not, the ‘something’ is a new prescription. According to Rita Redberg, editor in chief of JAMA Internal Medicine, people tend to prefer the idea of taking a pill more than making sweeping lifestyle changes like exercise or better diets, and in the case of a doctor suggesting adding a new drug, a senior is less likely to question their decisions.
A prescribing cascade.
The overuse of medications can cyclically be caused by medication itself, in a process called a prescribing cascade.[4] Here’s how that works: A patient taking a drug to treat high blood pressure may develop edema (or a collection of fluid in the body) for which they are then prescribed diuretics. The diuretic causes an overactive bladder, for which another drug is prescribed. This triggers dry mouth, which is treated with yet another drug, and the cycle continues. Each adverse drug reaction is misinterpreted as a problem in itself, leading to more prescriptions.
Unnecessary medications.
A lot of redundant drugs are prescribed to the elderly, often at the end of a hospital stay. David Reuben, chief of the geriatrics division at UCLA said, “There are a lot of souvenirs from being in the hospital: medicines they may not need.” Drugs prescribed within a hospital are often meant to treat the acute illness for which the patient was admitted. Others could be to prevent complications. Still others could be prescribed to prevent side effects of the aforementioned drugs. “It’s very typical to see a patient who has a few episodes of reflux and is then put on a PPI (proton pump inhibitor) and a few years later are still taking it,” says Ranit Mishori, a professor of family medicine at Georgetown University. Experts believe that drugs to treat acid reflux are not only overprescribed but can also be linked to fractures and dementia with long-term use.[5]
All in all, doctors keep adding to an existing list of medications, and seniors return home uncertain about how long they have to take it. Considering the fact that seniors are also more prone to dementia and forgetfulness, the burden of monitoring drug intake can often be too much to handle.
Fragmentation of care.
Seniors often see more than one physician and fail to share this information, which has led to a rampant lack of communication between one person’s several care providers. Even if a patient does share their existing prescriptions, “there is a reluctance to tinker or change things too much,” according to the University of Michigan geriatric psychiatrist Donovan Maust. Clinicians believe that if a patient has been on a certain drug, their previous care provider probably prescribed it for a good reason.
How can polypharmacy be reversed or reduced?
Hospitals and physicians have a couple of options when it comes to reducing drug intake among seniors.
Hire a specialist.
The inpatient geriatrics division at UCLA Medical Center in Santa Monica is a good example of what a designated specialist can do. Their hire in question is Dominick Bailey, a clinical pharmacist specializing in geriatric care. One of the main goals of the geriatric center has been to make sure that seniors are not harmed by drugs meant to help them. Bailey’s primary focus within this has been to improve care and reduce readmissions. Studies suggest that having someone like Bailey on board can bring about a reduction in drug complications and hospitalizations.[6]
De-prescribing.
There is a grassroots movement in the works that has its origins in Canada and Australia called ‘deprescribing’. What it entails is the systematic discontinuation of drugs that are inappropriate, redundant or plain unnecessary. Efforts such as the Choosing Wisely campaign (which aims to foster better patient-caregiver dialogue to reduce unwarranted tests and treatments) have pushed deprescribing further in the United States.
One of the primary tools in deprescribing has been the Beers Criteria, a list of medications that could be harmful to geriatric patients. It includes dozens of drugs, including antidepressants and antipsychotics. Pharmacists like Dominick Bailey also regularly refer to the Beers list when making assessments.
Several geriatricians may also choose to begin every appointment with a review of medications. It’s clear that physicians are hesitant about discontinuing medications that previous doctors may have ordered, so one of the ways to combat this has been to require doctors to note why a medication has been prescribed. Surveys among doctors have found strong support for this practice too.
Another exercise that could potentially help is empowering patients with knowledge about their prescriptions. Patients often find, for instance, that they tried to stop taking a sleeping pill, couldn’t sleep an entire night, and hence resumed taking it. Patients like these would benefit from a doctor that had explained – at the time of prescribing – the mechanism of ‘rebound insomnia’, which typically only lasts 3-5 days.
Physicians looking to counter polypharmacy may come up against significant challenges, not the least of which is the pressure from pharmaceutical companies to make profits. In the wake of the USA’s prescription epidemic, several states have implemented PDMPs or Prescription Drug Monitoring Programs. These aim to reduce prescription drug abuse or diversion. What may also help is a closer look at substances currently demonized by Big Pharma – CBD, for instance – as possible non-addictive alternatives in geriatric care.
[1]https://www.tandfonline.com/doi/full/10.1517/14740338.2013.827660
[2]https://www.ncbi.nlm.nih.gov/pubmed/28784299
[3]https://lowninstitute.org/wp-content/uploads/2019/08/medication-overload-lown-web.pdf
[4]https://www.meded101.com/3-classic-examples-of-the-prescribing-cascade/
[5]https://www.acphospitalist.org/archives/2016/03/unnecessary-PPIs.htm